What was the challenge?
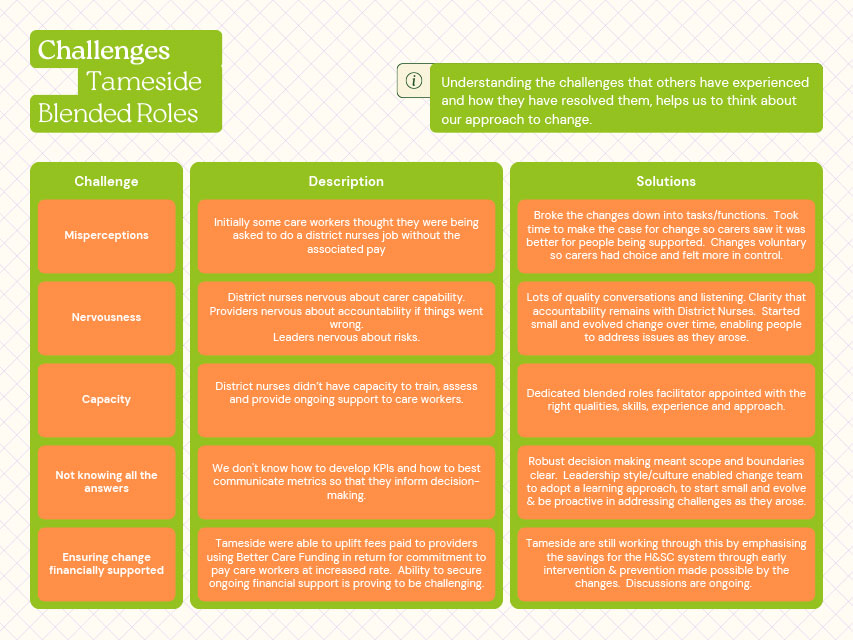
Recruitment and retention in homecare were ongoing challenges for providers. Local commissioners identified also identified the lack of clear career progression in social care.
What did you do?
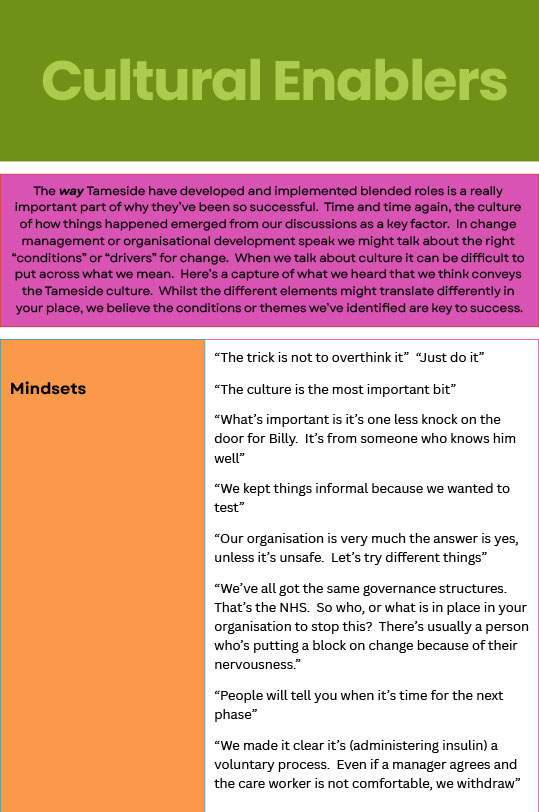
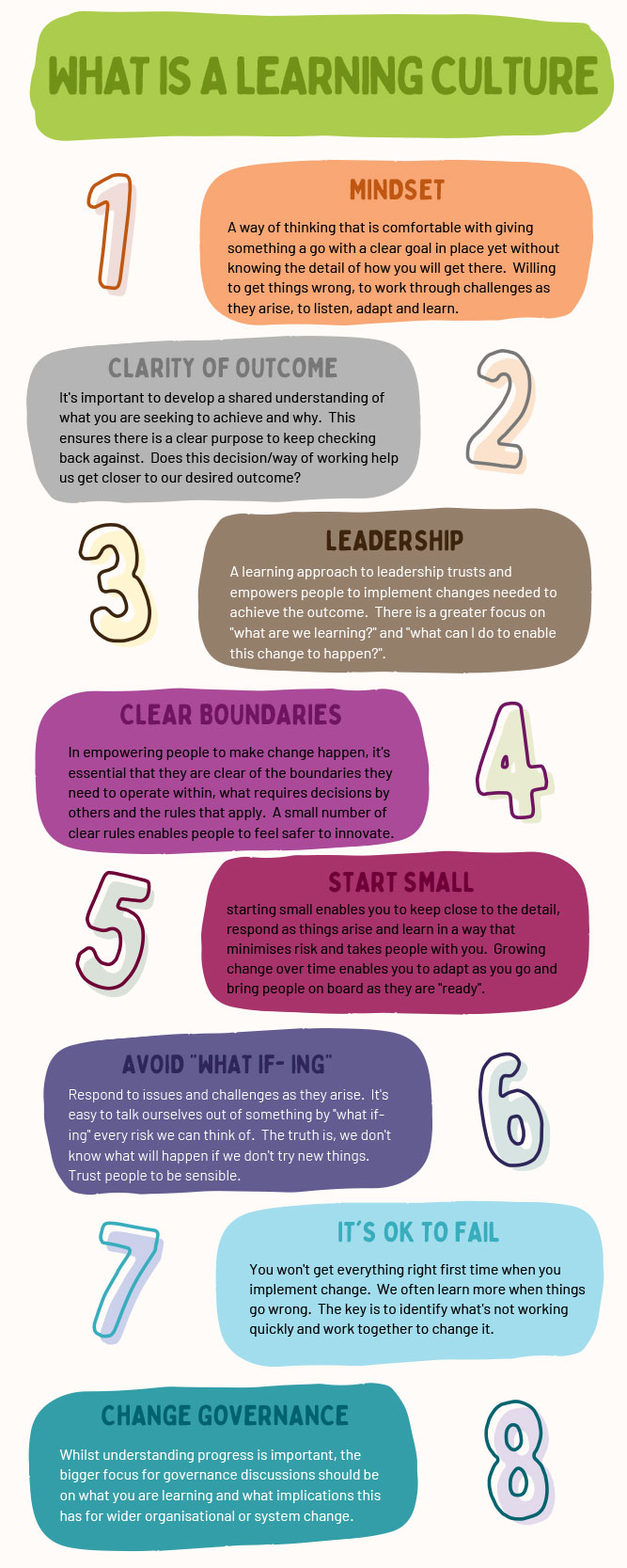
Tameside Council wanted to test whether bringing low level healthcare tasks into the remit of social care roles would improve care, and change how social care perceived.
How did you do it?
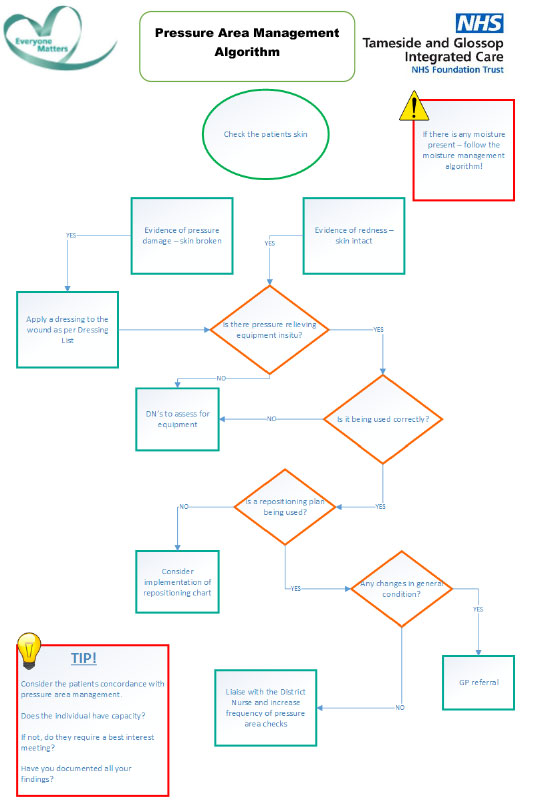
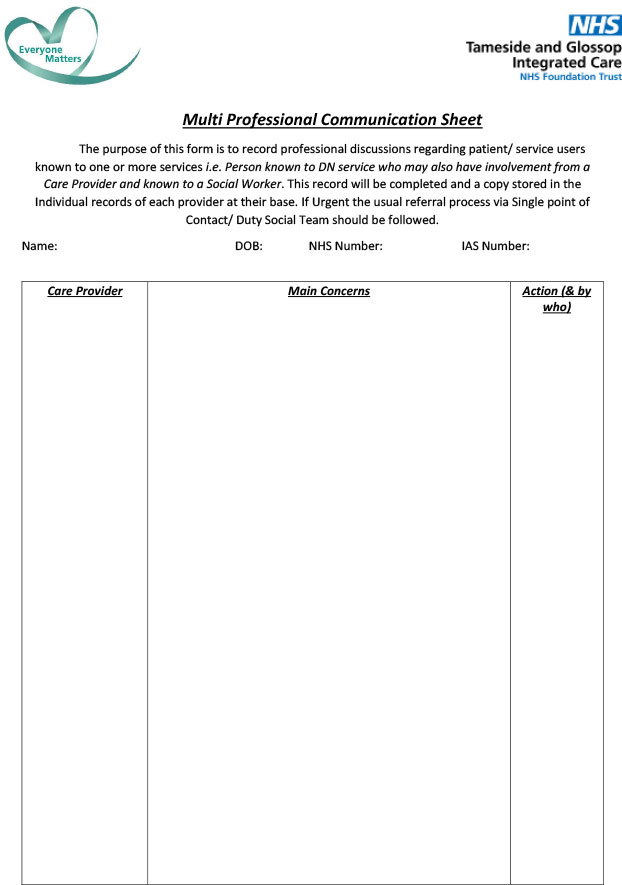
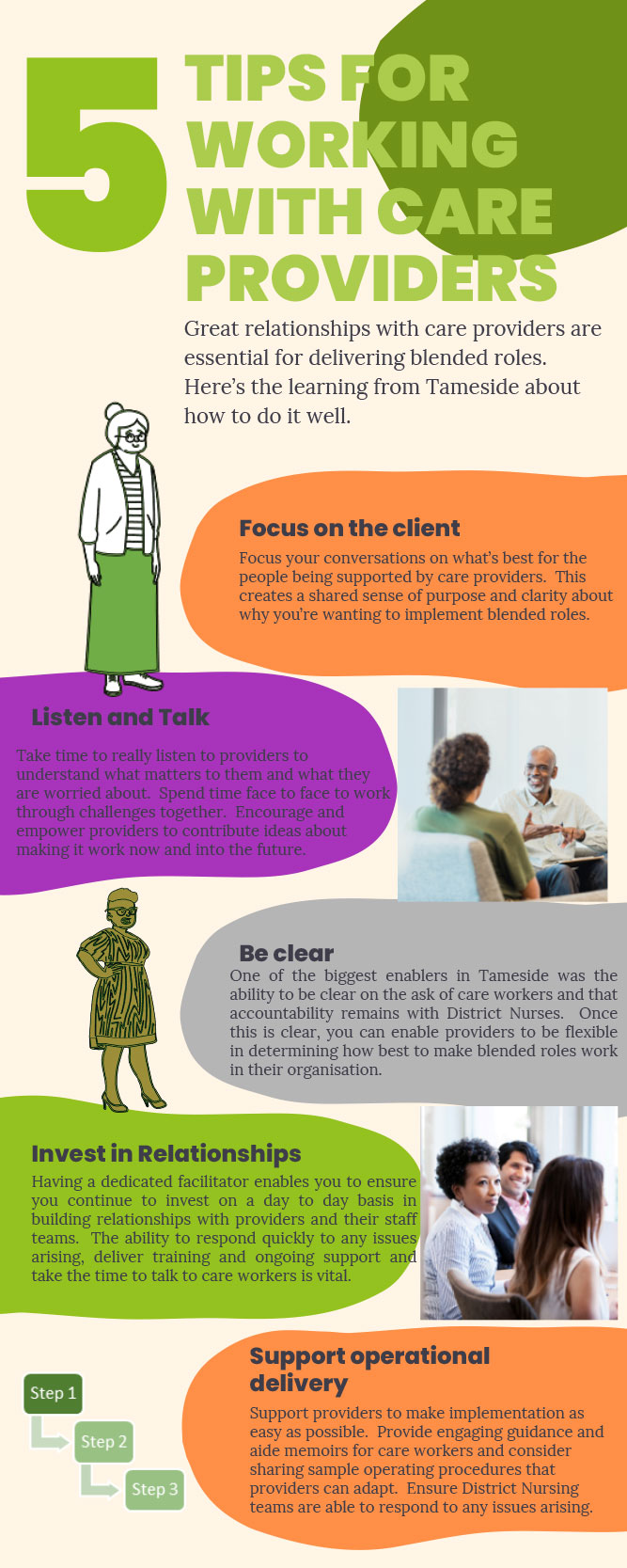
Commissioners built on close working relationships with interested providers and reached out to District Nurses. Together they agreed to link additional tasks to increased hourly rate. This was tested first and then rolled out to all homecare workers. Training was initially provided by District Nurses, with a Co-Ordinator then recruited to manage and deliver training.
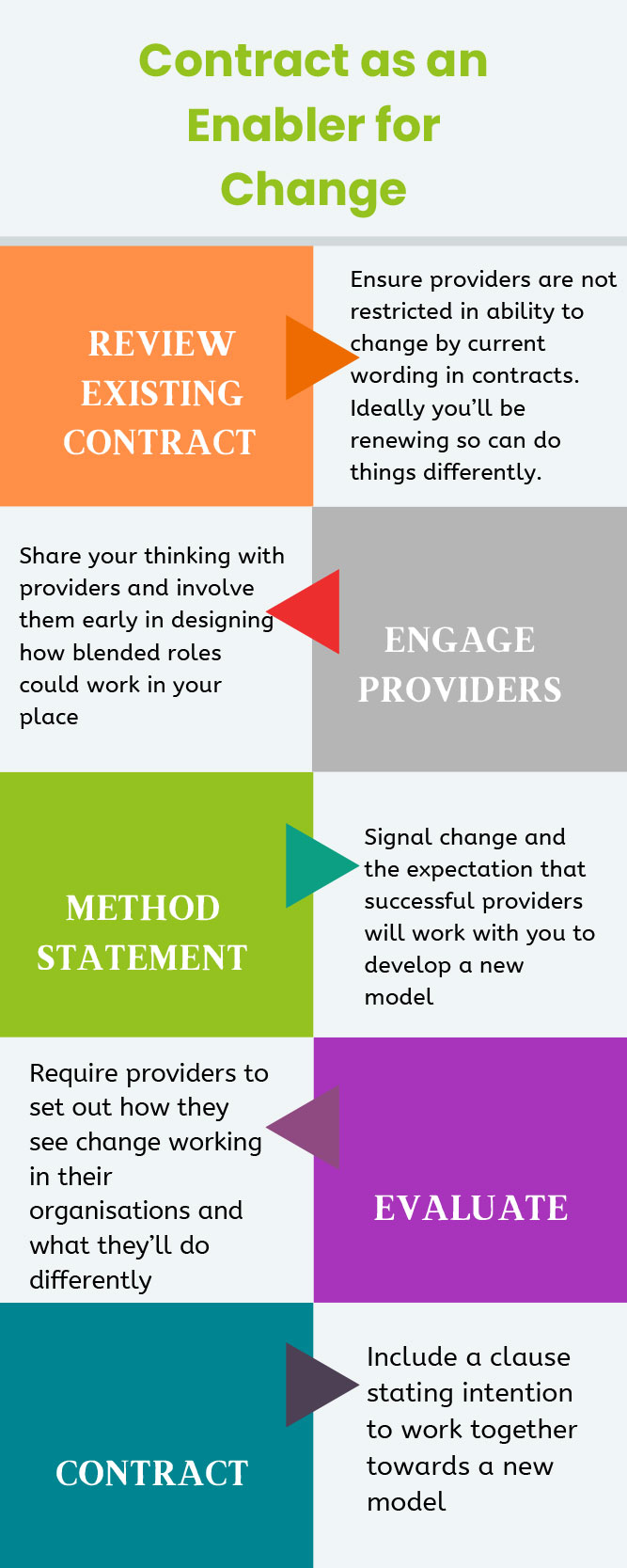
Engaging with the blended roles approach has been a contractual requirement for five Support at Home providers since June 2023 and for care homes over a similar period. Currently, in the region of half a dozen care homes are involved although numbers fluctuate over time. Support at Home providers have been involved in the delegation of low level health care tasks since 2019 under the previous contract.
Blended roles was addressed specifically in the Support at Home tender most recently and previously was part of a developmental spec wherein Tameside outlined what was wanted to do without knowing how we would do it. Buy-in from providers was ensured as a result. Our FPS (framework) home care providers are not required to engage with the approach.
From an ASC perspective, this was approached with a view to addressing issues around continuity of care, recruitment and retention and career progression for providers and improving provider integration in the neighbourhood teams.
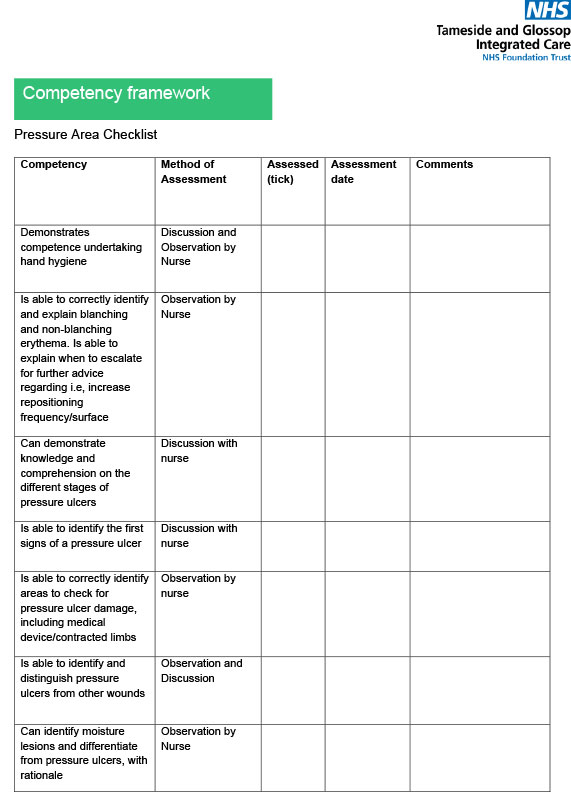
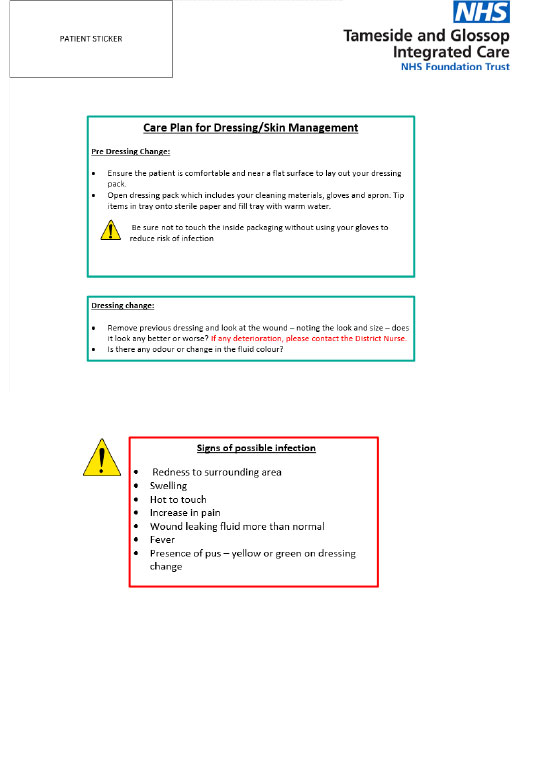
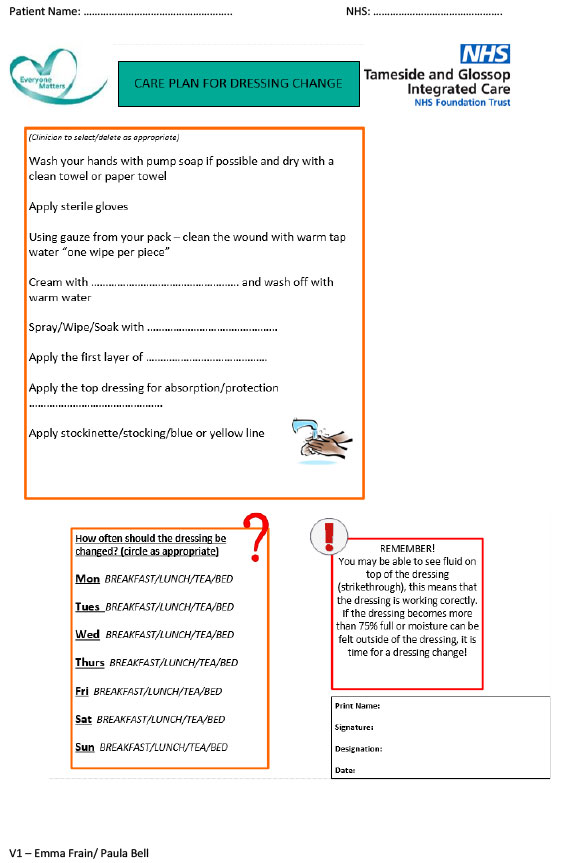
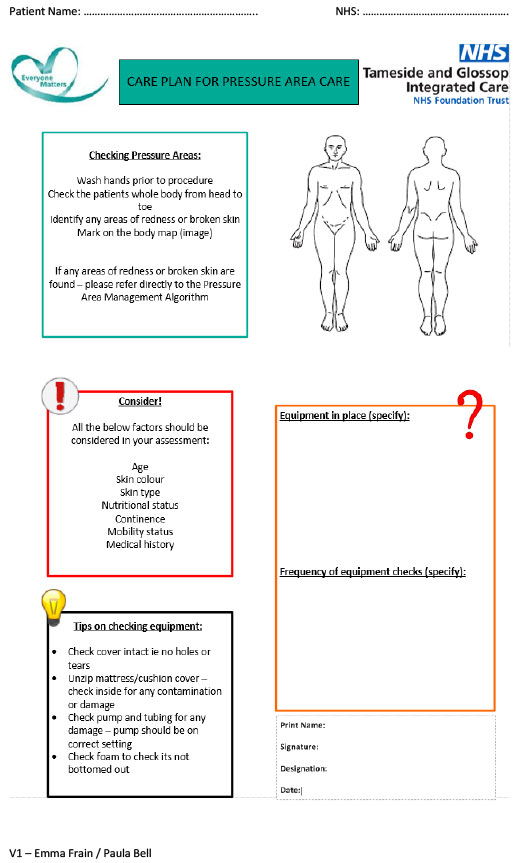
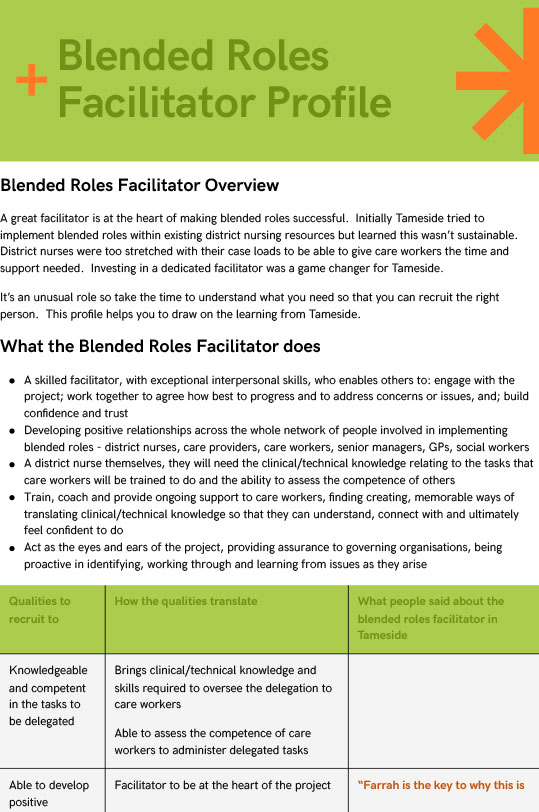
A Blended Roles Facilitator works closely with providers in terms of delivering training, identifying shared care and signing off carers as competent.
What went well?
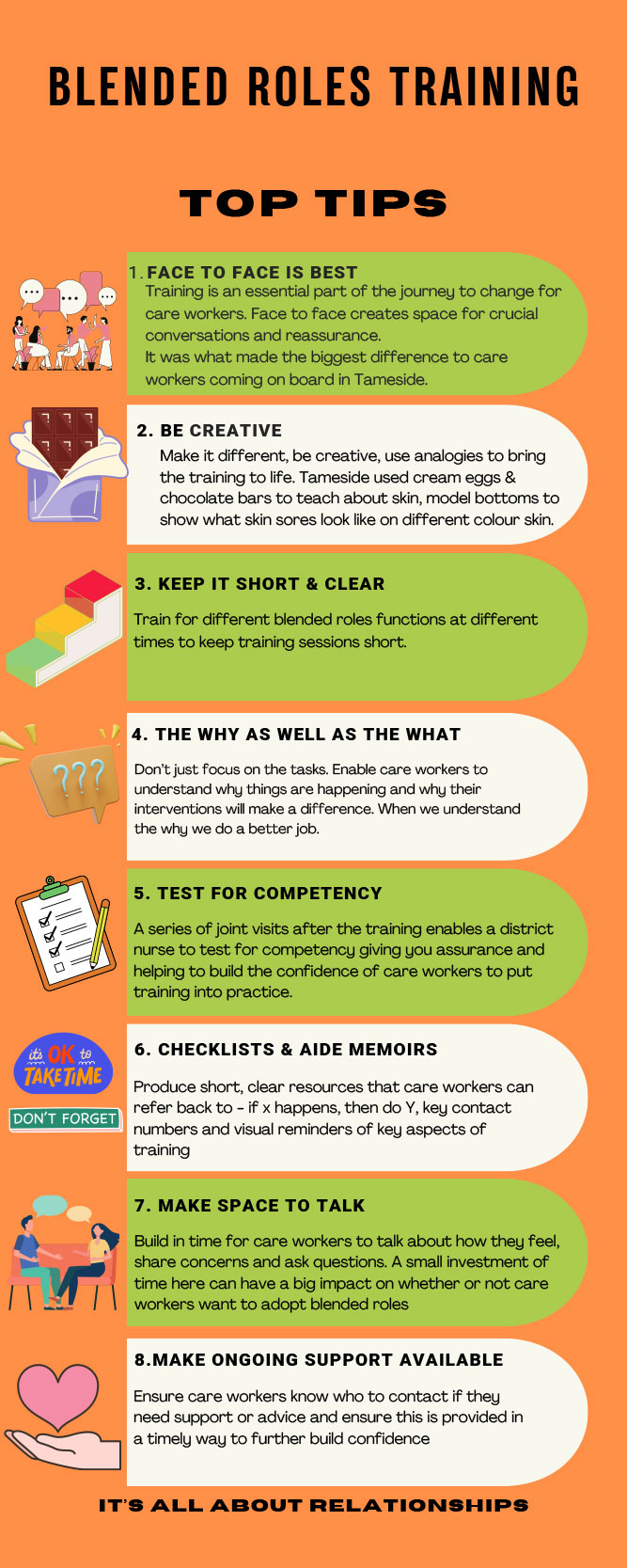
Staff really like the approach and it makes demonstrable impact on care people receive. The approach taken “meets people where they are at” e.g. more hesitant staff able to sit in on training to appease fears. An interactive style of training is used, e.g. cream egg to teach skin composition.
Total number of patients delegated for insulin administration (Year July 2021 – Dec 2023) = 25
Current number of patients delegated for insulin (last updated 14.02.24) = 11
Number of carers actively administering (last updated 14.02.24) = 12
Total number of carers trained: 30+
Number of Domiciliary care Providers = 5
Initially, 1/6 providers agree to blended roles. Since then we now have 5 providers, and all 5 are involved.
What challenges did you encounter along the way
Providers were not originally keen to do insulin administration. It was agreed not to include initially but incorporated as confidence and training processes developed. Some staff initially hesitant about accessing training, and district Nurse capacity to deliver training was an issue (addressed by appointing a dedicated Co-Ordinator).
What did you learn?
The resources within this Blueprint focus on the wider learning. Key points include the importance of recruiting a co-ordinator to deliver training and support, which was not sustainable using District Nursing capacity. This approach freed up District nursing capacity to focus on more complex work. The project has had a very positive impact on joint working between social care and District nurses. Particular documents were key, e.g. a competency sign-off booklet. Importantly, “show not tell” was key in ensuring buy-in.
What can the wider system learn from your experiences?
This approach is better for residents – with more continuity of care, less people knocking on door: Helps with infection control. District nurses are very supportive. The impact is so much more than administration of tasks , with a major impact on quality of relationships and joint working between care workers and District Nurses. Much more communication provides the ability to intervene early.